Living with spinal stenosis can make everyday movements—like walking, standing, or even sleeping—painful and frustrating. This condition, often related to aging or spinal degeneration, can lead to nerve compression, numbness, and loss of mobility if left untreated. At the Center for Regenerative Therapy & Pain Management, we offer advanced, non-surgical solutions that target the source of your pain and help you regain control of your life.
Spinal stenosis is a condition that occurs when the spaces within your spinal column become narrowed, putting pressure on the spinal cord or nerves. This compression can cause pain, numbness, tingling, or muscle weakness in the back, neck, or limbs. The two most common forms are cervical stenosis (affecting the neck) and lumbar stenosis (affecting the lower back). Though often associated with the natural aging process, spinal stenosis can progress over time. Fortunately, there are safe, effective, non-invasive treatments available to relieve symptoms and improve your quality of life.
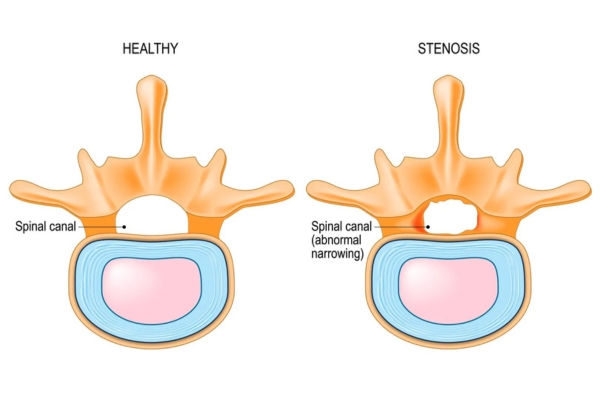
As spinal discs lose hydration and elasticity with age, they become thinner and less effective at cushioning the vertebrae. This shrinkage can lead to narrowing of the spinal canal and increased pressure on the nerves.
With age, the ligaments that support your spine can thicken and become less flexible. In some cases, they bulge into the spinal canal, contributing to reduced space for nerves and increased discomfort.
Some people are born with a naturally narrower spinal canal, making them more susceptible to developing stenosis later in life—even with minimal degenerative changes.
A disc that bulges or ruptures may protrude into the spinal canal and press directly on nearby nerve roots. This mechanical compression is a frequent trigger for symptoms like radiating pain or weakness.
Osteoarthritis in the spine can cause bone overgrowth, known as bone spurs. These protrusions take up space in the spinal canal and may compress nerves, particularly in the lower back or neck.
Fractures, dislocations, or trauma to the spine can alter spinal structure and lead to narrowing of the canal. Even after healing, swelling or scar tissue can continue to affect nerve function.

Symptoms vary based on where the stenosis occurs, but most result from nerve compression that disrupts movement and comfort:
Pain in the back, neck, or limbs
Numbness or tingling in arms or legs
Weakness or heaviness in limbs
Pain worsening while walking or standing
Relief with sitting or leaning forward
We begin by reviewing your medical history and understanding the nature of your symptoms. A physical and neurological exam helps evaluate mobility, balance, and nerve involvement. Imaging such as an MRI or CT scan confirms spinal narrowing. In some cases, diagnostic injections are used to precisely isolate the source of pain.
These image-guided injections deliver powerful anti-inflammatory medication directly into the epidural space of the spine. By reducing swelling and irritation around the spinal nerves, they help relieve pain, improve mobility, and support long-term symptom management.
Nerve blocks involve injecting a local anesthetic near specific spinal nerves to interrupt pain signals. They not only provide temporary relief but also serve as a diagnostic tool to help identify the exact source of nerve-related discomfort in spinal stenosis patients.
This minimally invasive procedure uses heat from radio waves to target and disable pain-generating nerves. It is particularly effective for long-standing back or neck pain caused by stenosis, offering months of relief without the need for ongoing medication.
A small implanted device delivers low-level electrical signals to the spinal cord to disrupt pain messages before they reach the brain. It is ideal for patients with chronic spinal stenosis symptoms who haven’t found relief from other treatments.
These injections target painful knots of muscle—often in the back, neck, or shoulders—that contribute to nerve compression. By relaxing these tight areas, trigger point injections reduce localized pain and improve spinal alignment and comfort.
Customized physical therapy programs help strengthen the muscles supporting the spine and correct postural imbalances. This treatment improves stability, increases flexibility, and prevents further narrowing of the spinal canal over time.
Spinal stenosis symptoms often worsen without treatment—getting care early can prevent long-term nerve damage.
Persistent pain or weakness in the back, neck, or limbs
Trouble walking long distances or standing upright
Loss of coordination or balance
Pain relief only when sitting or leaning forward
Symptoms no longer improving with home care

Spinal stenosis can make everyday activities—like walking, standing, or even resting—feel like a challenge. But you don’t have to live with constant pain or numbness.
Our team provides personalized, image-guided treatments designed to relieve nerve pressure and restore your mobility—without the need for surgery.
Spinal Stenosis
Spinal stenosis is the narrowing of the spinal canal, which places pressure on the spinal cord or nearby nerves. This can lead to symptoms like pain, numbness, tingling, and muscle weakness. It most commonly affects the neck (cervical stenosis) or lower back (lumbar stenosis).
Severe spinal stenosis involves significant narrowing that leads to consistent nerve compression and noticeable loss of mobility or function. It may cause weakness, difficulty walking, or loss of bladder or bowel control. These cases often require urgent evaluation to prevent permanent nerve damage.
Most cases are treated non-surgically using options like epidural steroid injections, nerve blocks, physical therapy, or radiofrequency ablation. These methods aim to reduce inflammation, relieve pressure, and restore movement. Surgery is typically reserved for cases that don’t respond to conservative care.
While spinal stenosis is most often caused by age-related degeneration, genetics can play a role. Some individuals are born with a naturally narrow spinal canal, increasing their risk of developing symptoms later in life. This congenital form may show up earlier and progress faster.
Yes, in severe cases, spinal stenosis can compress nerves that control bladder and bowel function. This is considered a medical emergency known as cauda equina syndrome. If you experience sudden incontinence or numbness in the saddle area, seek immediate medical attention.
Yes, spinal stenosis can cause referred pain that radiates into the hips, buttocks, or thighs. This happens when compressed nerves in the lower back affect surrounding areas. Many patients mistake this for hip joint issues when it’s actually spine-related.
Cervical spinal stenosis (in the neck) can sometimes cause dizziness or a feeling of imbalance. This may result from disrupted nerve signals or reduced blood flow due to neck positioning. A thorough evaluation helps rule out other causes and determine if spinal stenosis is contributing.
Spinal stenosis is usually a progressive condition, especially if left untreated. Symptoms can worsen gradually, leading to greater pain, weakness, or numbness. However, early diagnosis and proper treatment can significantly slow progression and improve quality of life.

We provide advanced, personalized pain management care for patients across New Jersey, led by board-certified specialist Dr. Shane Huch.
Center for Regenerative Therapy and Pain Management © All Rights Reserved | A Division of Toms River Anesthesia Associates